Rezumat
Introducere. Limfedemul reprezintă o acumulare interstițială regională excesivă de lichide bogate în proteine. Poate fi primar, cauzat în principal de hipoplazia congenitală (boala Meige) sau de agenezia vaselor limfatice (boala Milroy). Infecțiile, malignitățile, staza venoasă cronică, radiațiile ionizante, obezitatea și insuficiența cardiacă congestivă reprezintă cauze comune ale limfedemului secundar. Deși tuberculoza cutanată poate fi însoțită de limfangită, asocierea acesteia cu limfedemul cronic este rar menționată în literatura de specialitate.
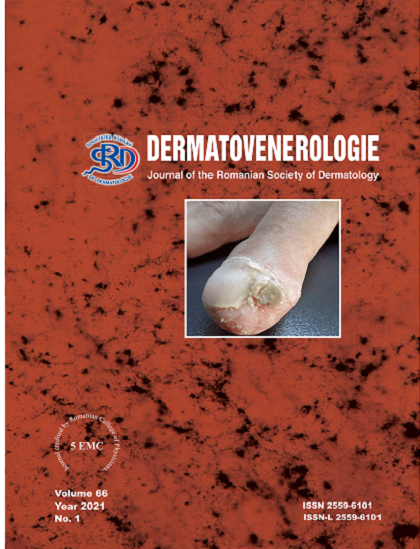
Caz clinic. Bărbat, în vârstă de 70 de ani, s-a spitalizat în Clinica Dermatologie pentru edem permanent, indurat și infiltrat la nivelul membrului inferior drept, cu tegument acoperit de papule translucide. De asemenea, pacientul prezenta în regiunea calcaneană dreaptă o formațiune keratozică, aspră la palpare, 1,5 cm diametru, cu ulcerație centrală (aspectul clinic sugerează o tuberculoză verucoasă). Din istoric reținem că, în urmă cu 7 ani, după o înțepătură la nivel calcanean drept, s-a format un abces care a fost chiuretat în serviciul Chirurgie, dar care a recidivat. După aproximativ 6 luni, membrul inferior drept a început să crească în diametru prin edem important. Pentru limfedemul cronic, pacientul a urmat, anterior spitalizării, tratament cu Detralex, Pentoxi Retard, Vessel Due F, fără rezultate notabile. Examenul histopatologic a pledat pentru diagnosticul de Tuberculozã cutanată. Investigațiile au exclus o tuberculoză viscerală, iar Echo Dopplerul nu a evidențiat patologie venoasă sau arterială. S-a instituit tratament specific cu tuberculostatice (Izoniazidă 300mg, Rifampicină 600 mg, Pirazinamidă 2000 mg, Etambutol 1600 mg 7/7) cu o durată de 9 luni, evoluția fiind favorabilă, cu dispariția formațiunii verucoase de la nivel calcanean drept, diminuarea limfedemului și dispariția papulelor de la nivelul membrului inferior drept.
Discuții. Tuberculoza verucoasă cutanată (TVC) reprezintă cea mai frecventă formă de tuberculoză exogenă paucibacilară. Este rezultatul inoculării primare la persoane anterior sensibilizate la tuberculină, care mențin imunitate moderată până la ridicată împotriva M. tuberculosis. Este vorba fie de autoinoculare, fie heteroinocularea în urma unui contact accidental sau profesional. Infecția bacteriană secundară și limfedemul cronic sunt posibile complicații ale leziunilor extinse care afectează de obicei extremitățile. TVC poate să persiste mulți ani dacă nu este tratată corespunzător. De obicei, există un răspuns favorabil la terapia antituberculoasă, asemenea cazului nostru.
Concluzii. Limfedemul cronic asociat tuberculozei verucoase poate fi remis prin tratament de durată cu tuberculostatice. Diagnosticul și tratamentul precoce al tuberculozei cutanate sunt esențiale pentru reducerea complicațiilor.