Introduction. Leukemia cutis is a rare cutaneous
leukemia-specific manifestation and is characterized by
infiltrates with paraneoplastic leukocytes or their
precursors located in the dermis, subcutaneous tissue,
cutaneous annexes and blood vessels. Several terms have
been used to describe the various leukemia cutis manifestations
in acute myeloblastic leukemia: the granulocytic
sarcoma, the monocytic sarcoma, primary extramedullary
leukemia and the chloroma.
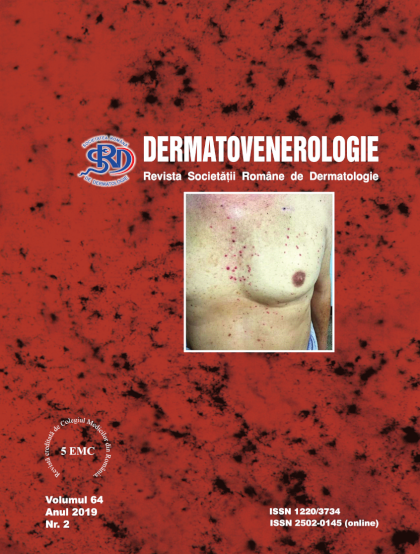
Clinical case. A 65-year old man from the urban area
under evidence of the Hematology Department since
August 2018 for acute promyelocytic leukemia (AML-M3
in the FAB classification) was consulted in the Craiova
Dermatology Department in January 2019 for several
nodular tumor masses that were firm, reddish, of 0.2-2 cm,
well defined, located in the left inguinal, lumbar, anterior
thorax and scalp areas. The tumor masses appeared 3 weeks
ago. The patient received remission induction therapy with
cytarabine, idarubicin and all-trans retinoic acid (ATRA),
obtaining complete remission (blasts 2-3%), then he
continued with consolidation treatment with cytarabine,
epirubicin and ATRA. The histopathological aspect and the
immunohistochemical staining are compatible with a
myeloid sarcoma (extramedullary determination of acute
myeloblastic leukemia). The immunophenotyping from
marrow aspirate, repeated in the Hematology Department
in February 2019 suggested a diagnosis of acute
promyelocytic leukemia with positive residual disease
which means a relapse. The cutaneous lesions have
regressed after hematologic retreatment, with some leftover
pigmented spots on the torso. The patient is currently
under treatment with cytarabine.
Discussions. The incidence of cutis leukemia depends
on the type of leukemia, with a frequency of 2-18% of cases
in acute myeloblastic leukemia. The physiopathology that
underlies the leukemic cell migration to the skin is not clear.
Most cases of leukemia cutis in acute promyelocytic
leukemia that were described in literature were associated
with the use of ATRA, that is associated with a high
incidence of extramedullary diseases as relapse after
complete remission. There is the possibility that ATRA and
anthracyclines may not reach the places where extramedullary
infiltrates occur. Clinically, LC can look like
erythematous papules or nodules in 60% of cases. Because
of the unspecific clinical aspect of the skin lesions, the
cutaneous biopsy and the bone marrow biopsy are necessary
for establishing the diagnosis. The prognosis of patients
with LC is unfavorable, many also having other
extramedullary presentations of leukemia. The treatment of
leukemia cutis involves the treatment of the underlying
disease.
Conclusions.
Leukemia cutis is a skin marker of
hematologic malignant disease but it is a rare manifestation
in acute promyelocytic leukemia. Treatment with ATRA
can induce leukemia cutis occurrence. The correct diagnosis
of leukemia cutis creates the prerequisites for diagnosing the
systemic disease and highlights the leukemia relapse,
similar to our case.